The recommended dose of apixaban/Eliquis for the reduction of stroke risks in nonvalvular atrial fibrillation is 5 mg taken orally twice daily (Eliquis Prescribing Information 4/2021).
The dose shall be reduced to 2.5 mg taken orally twice daily, if two of the three following conditions exist:
The dose shall be reduced to 2.5 mg taken orally twice daily, if two of the three following conditions exist:
- age 80 years and older
- body weight less than 60 kg
- serum creatinine 1.5 mg/dL and more.
Therefore the prescription for a patient with age 72 years, 80 kg body weight and serum creatinine 2.4 mg/dL is 5 mg taken orally twice daily.
What however is the case if this patient presents with an acute bronchitis which shall be treated with clarithromycin? The prescriber information for apixaban/Eliquis tells that no dose adjustment of apixaban is needed although clarithromycin is classified as a combined P-gp and strong CYP3A4 inhibitor which usually should be avoided to be coadministered. Is under these circumstances a prescription without dose adjustment justified? It looks like this.
But what about the impact of the renal failure? Can that be neglected although 27% of administered apixaban is cleared through the kidneys?
But what about the impact of the renal failure? Can that be neglected although 27% of administered apixaban is cleared through the kidneys?
The prescriber information mentions furthermore that the enyzmes CYP1A2, 2C8, 2C9 and 2C19 make minor contributions to the metabolism of apixaban. What would be then the conclusion if the patient also is on the antidepressant fluvoxamine, which blocks CYP1A2, 2C9, 2C19, and CYP3A4 , partially in a strong way? Or if the patient is a CYP2C19 PM?
Many questions where the prescriber information gives hints but does not help to resolve the puzzle in a time saving manner to make a rational decision. Checking the situation with SCHOLZ Databank and its MDDI functions brings help and more clarity. It demonstrates that multiple mechanisms which impede metabolism and elimination of apixapan each with only a minor impact may add up to a substantial adverse effect. Elevated exposures to apixaban of about the 2-fold and more which should be avoided due to the increased risk of severe bleeding may be real-time assessed and become with one mouse click visible and transparent. The following table summarizes a listing of such MDDI assessments.
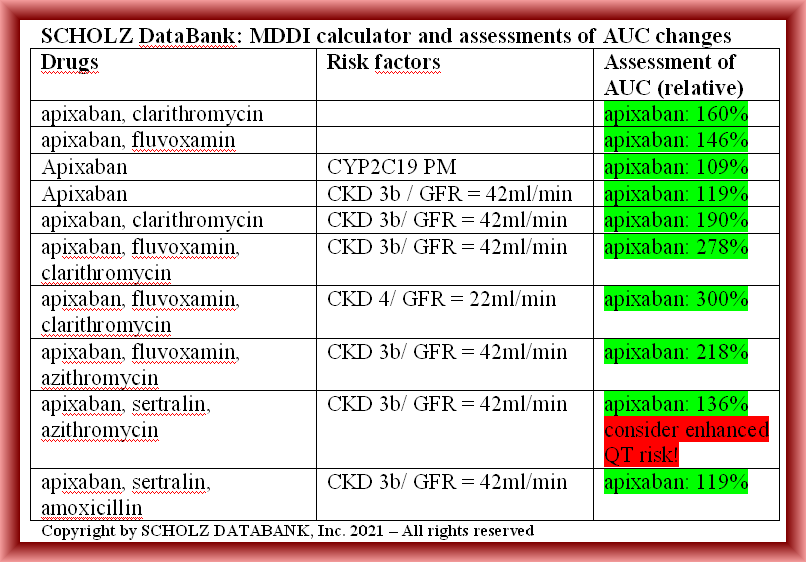
In particular, diverse alternate treatment scenarios with different or less risks may be retrieved within seconds, and if such alternatives generate new risks such as a prolonged QT interval, SCHOLZ DataBank provides you the appropriate alert, too. Look for example the scenario when combining apixaban with sertralin and azithromycin. And what concerns the introductory question if the apixaban patient with CKD 3b and a GFR of 42ml/min can be treated additionally with clarithromycin the answer is also clear: as the AUC of 190% is close to the treshold of the 2-fold it is recommendable to select a different antibiotic, for example amoxicillin.
Please contact us if you have any question or want to know how to get access to SCHOLZ DataBank and the MDDI technology when prescribing drugs for your patients!
Blog updated 05/05/2021