Patient Willy Nottingham is suffering from severe cardiac arrhythmia and is on the following
medication with Multaq/dronedarone, metoprolol, candesartan, simvastatin:
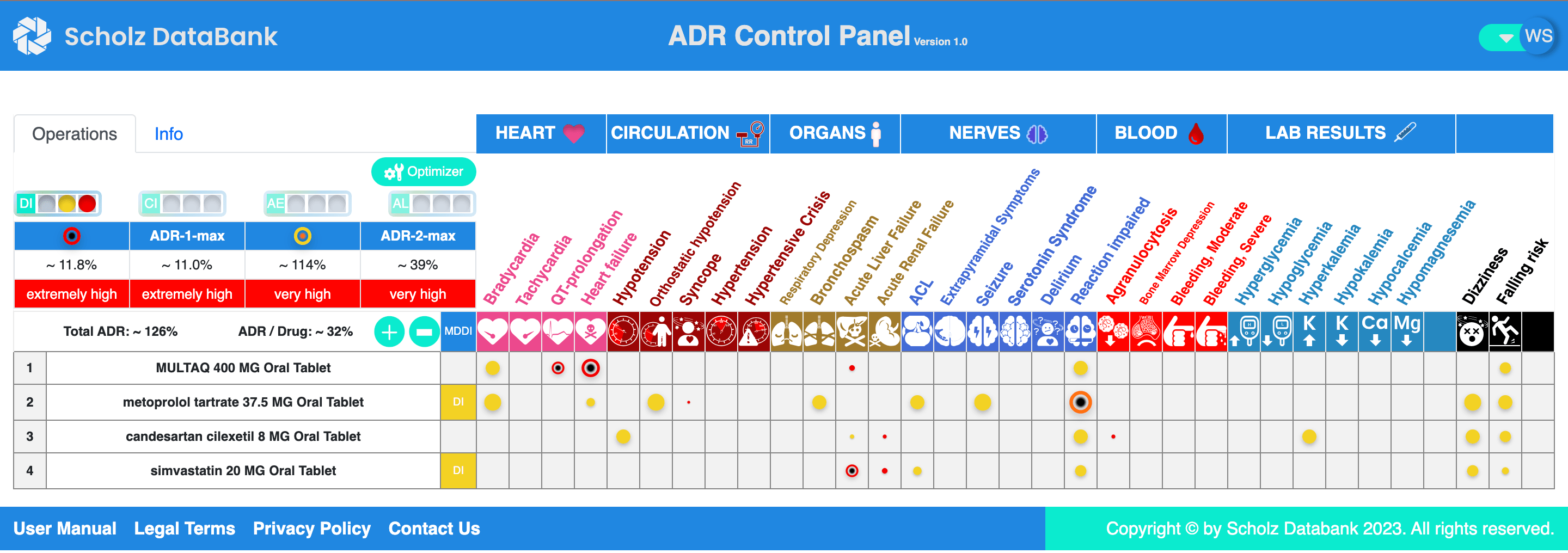
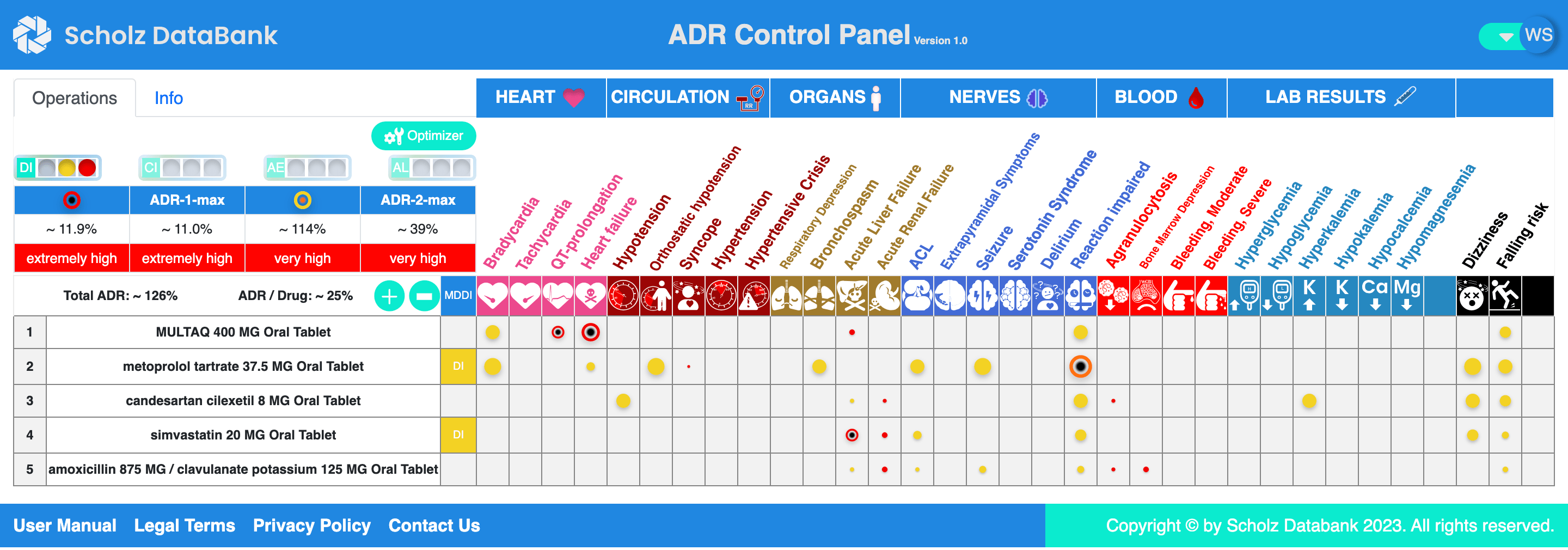
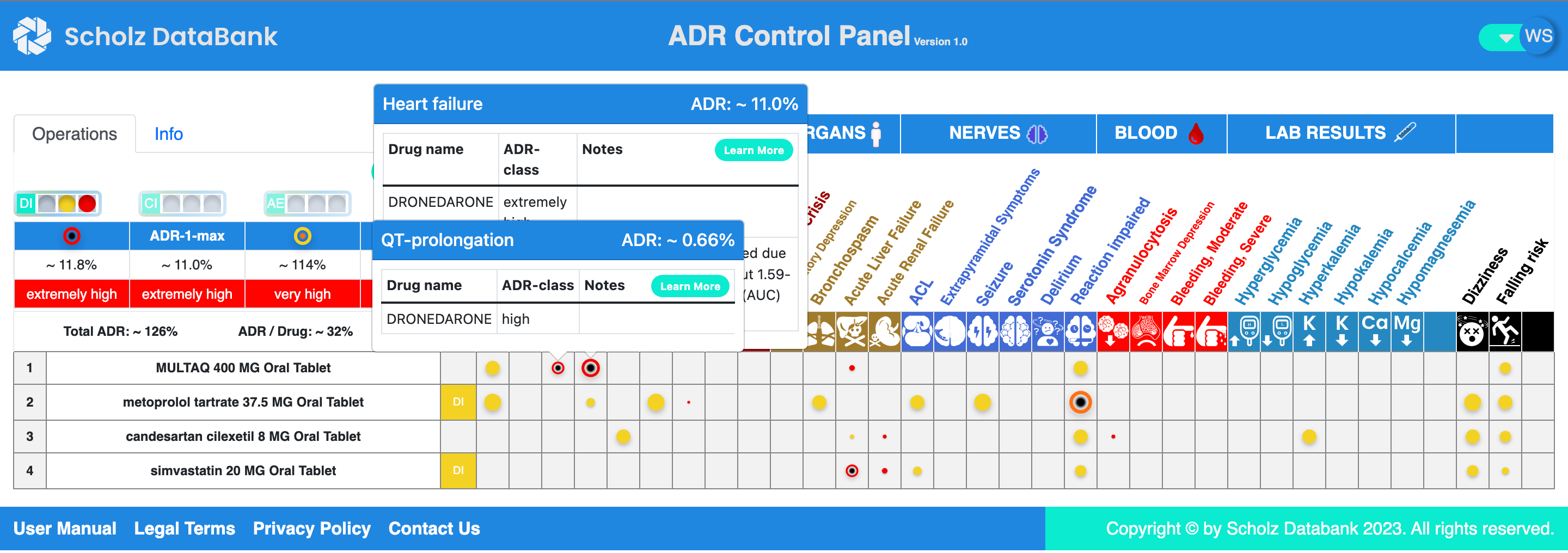
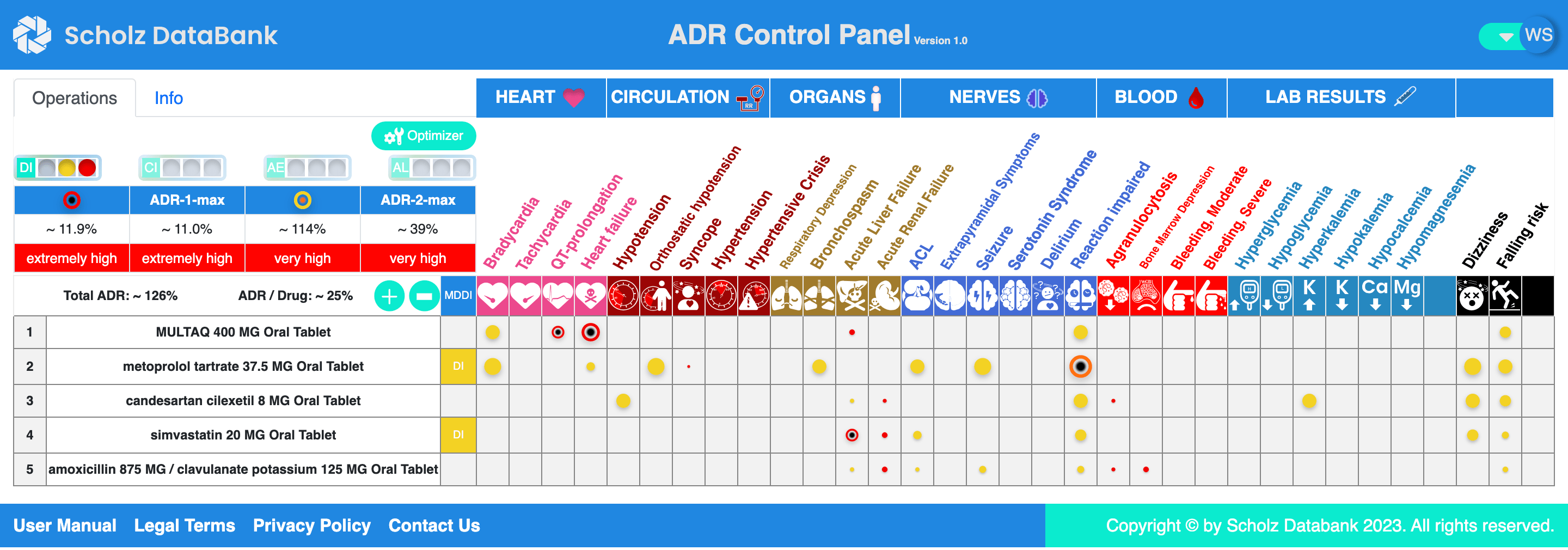
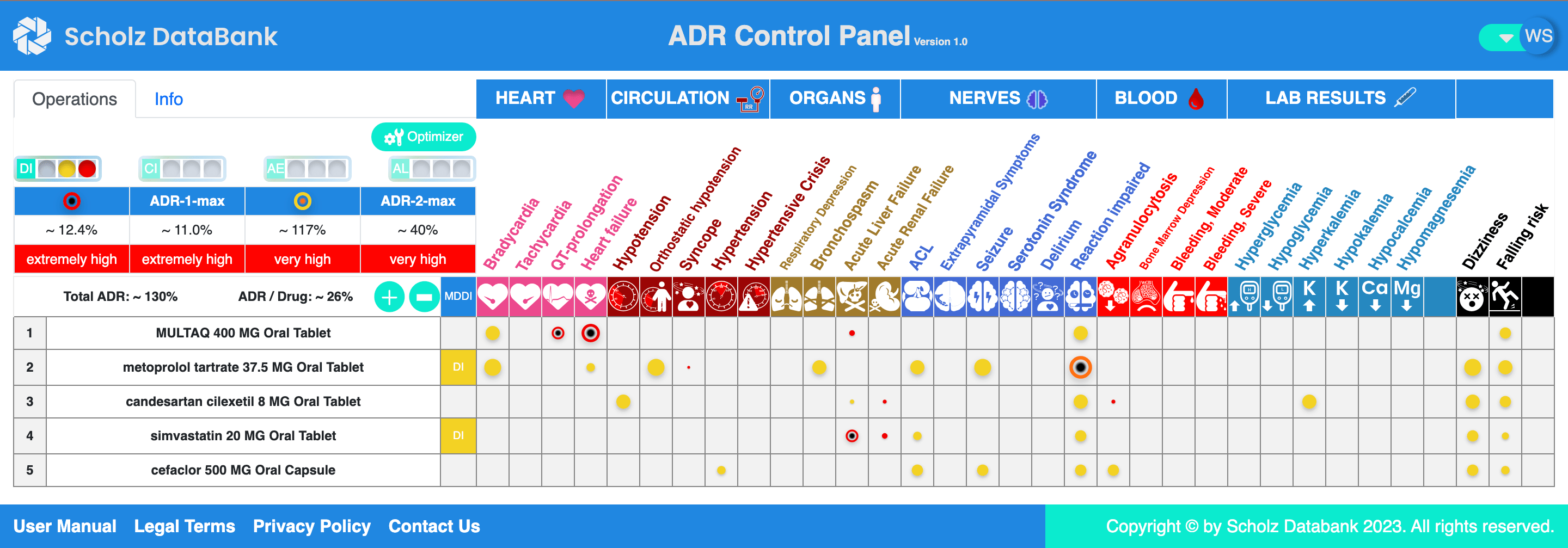
Dr. Meyer uses the ADR CP and is happy that he has stabilized the cardiovascular disease of Willy Nottingham with this medication and that he can overlook the major drug risks at one glance.
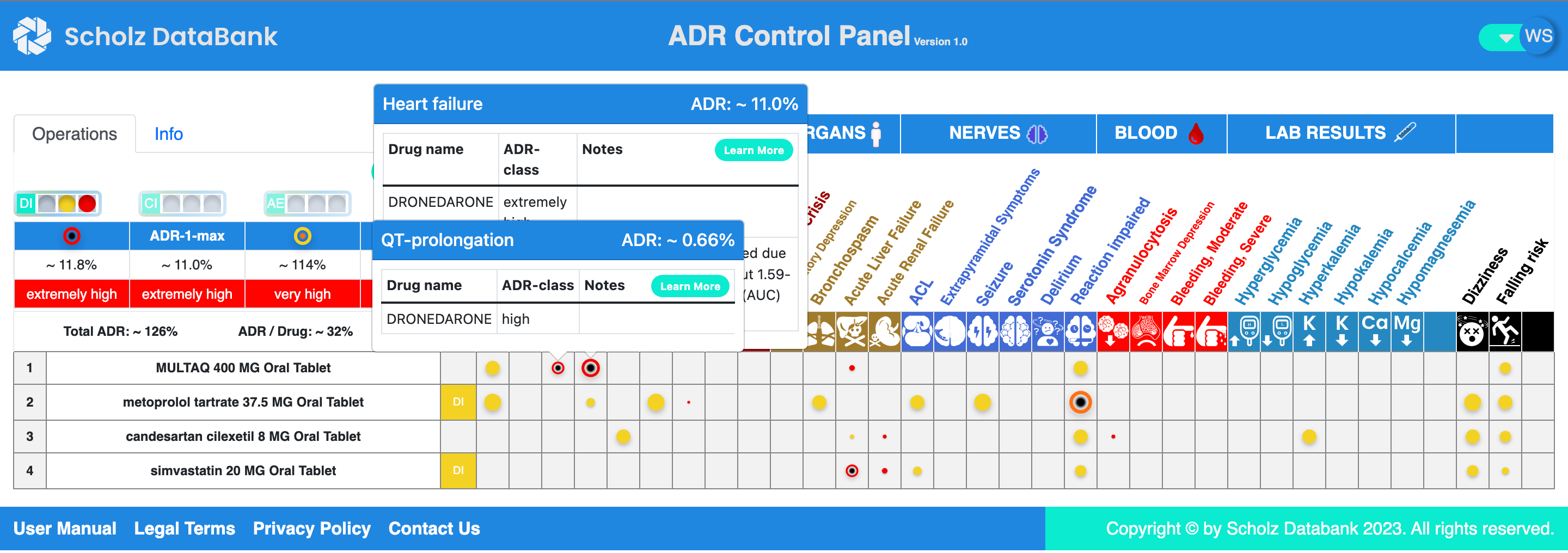
Willy Nottingham needs now an antibiotic due to a community acquired pneumonia diagnosed. Is clarithromycin appropriate? Or amoxicillin? Or Cefaclor? Is there any dangerous impact on the cardiac adverse risks which are already rather high and should not increase any more?
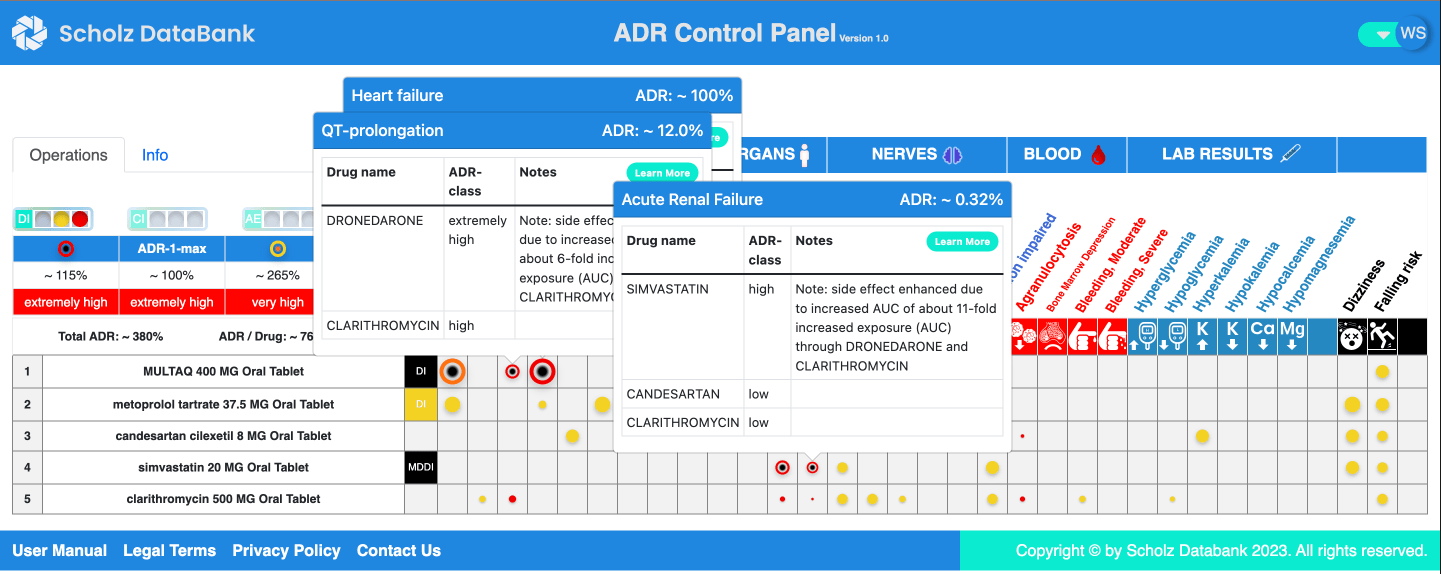
Dr. Meyer has abondened to waste his time working through long listings of pairwise potential drug drug interactions, for example when considering to prescribe clarithromycin.
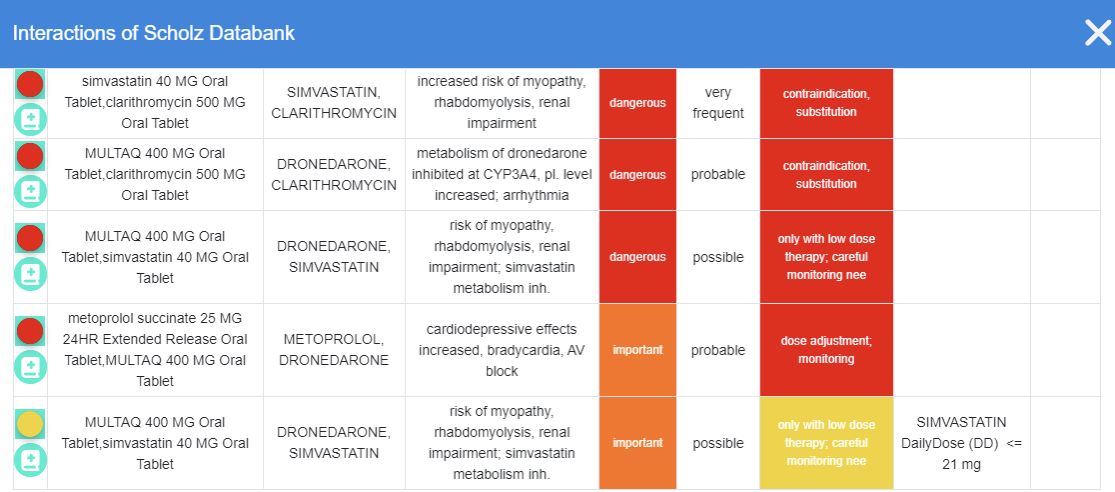
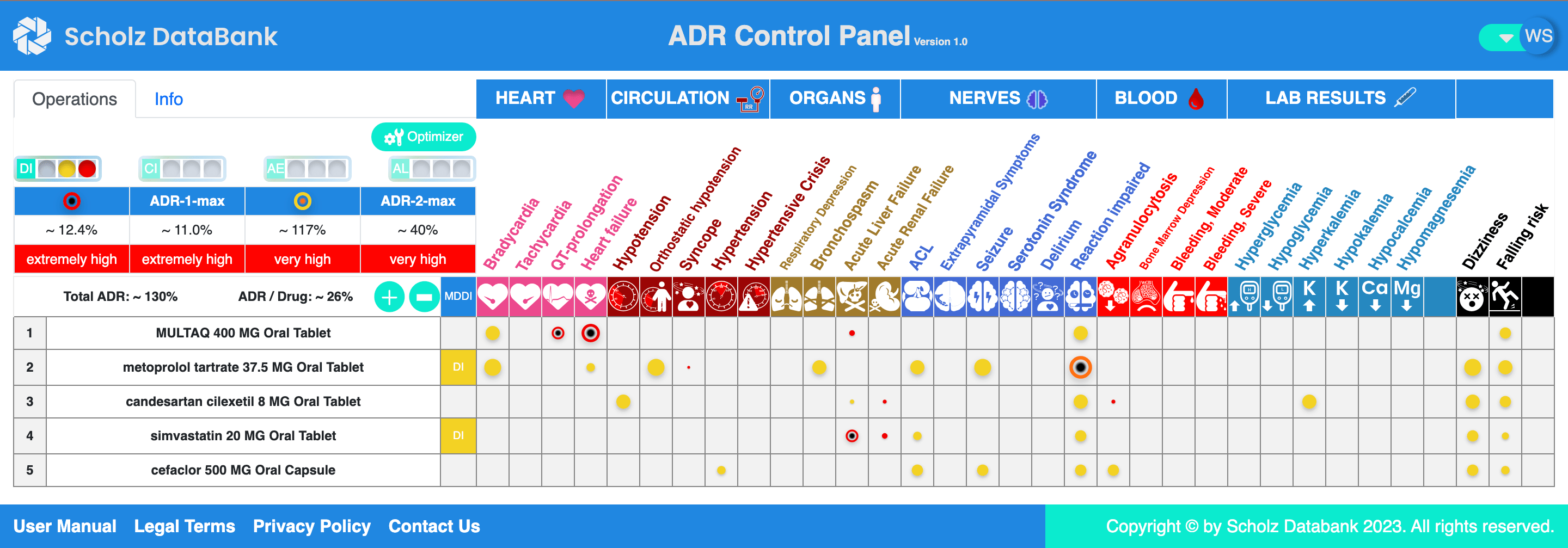
He just looks up and compares several ADR Control Panels without or with potential antibiotics to treat the pneumonia:
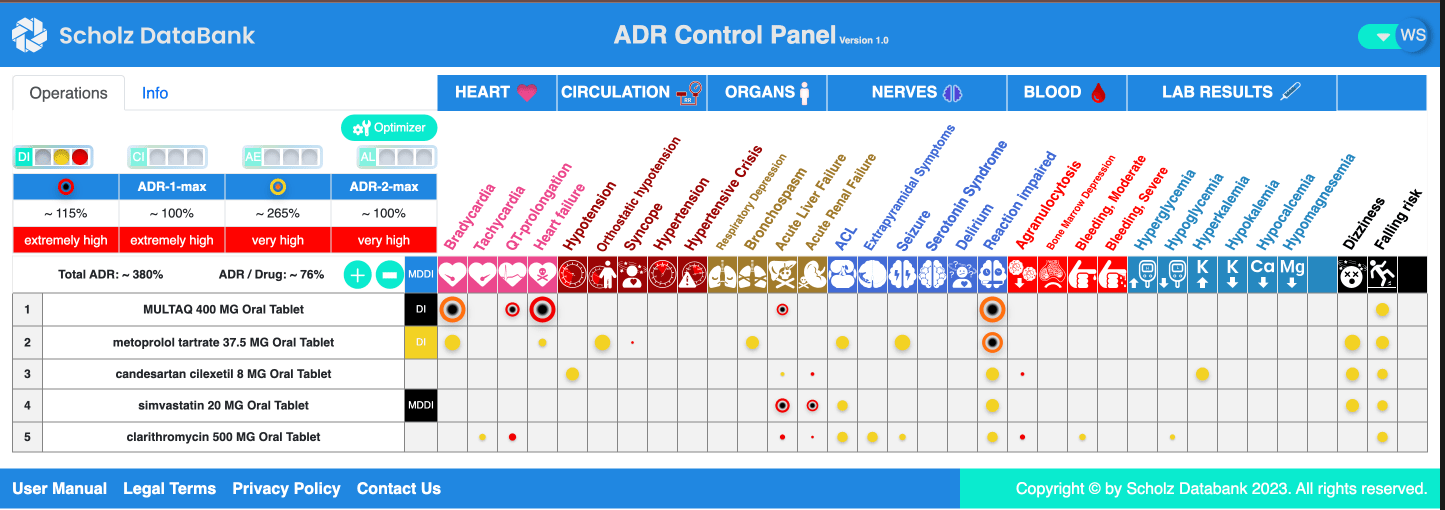
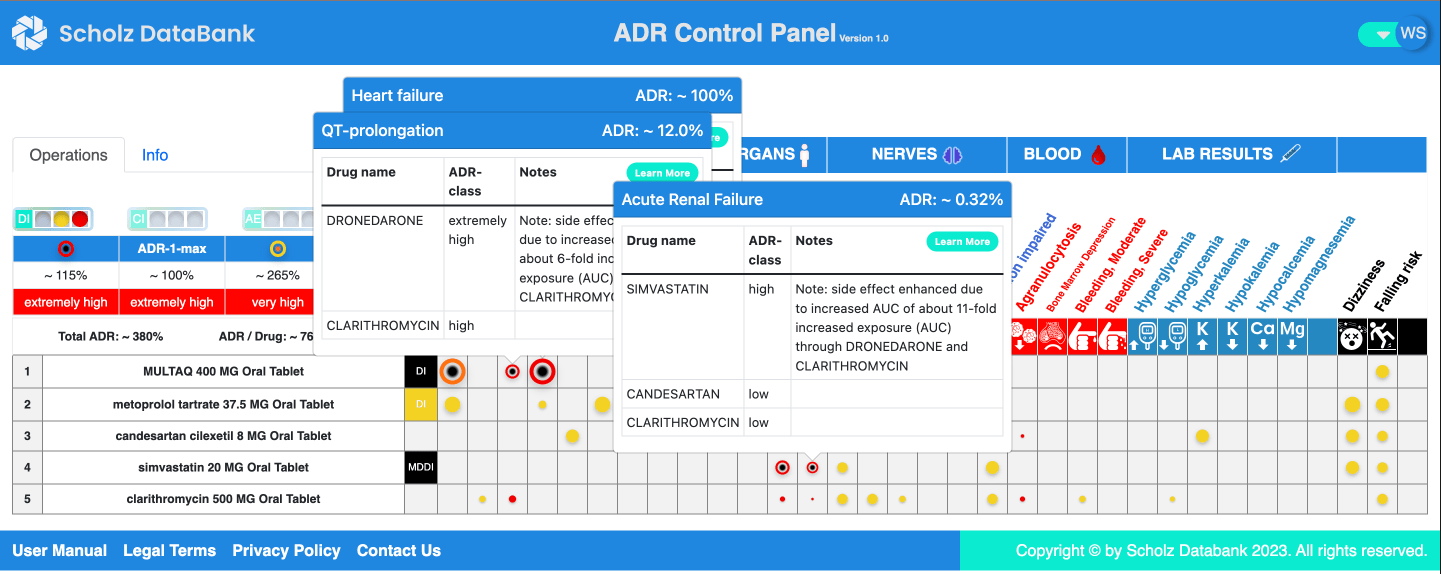
He realizes quickly the black MDDI alerts signalizing very hazardous kinetic drug drug interactions. The cardiac alerts for “QT prolongation” and “Heart Failure” emphasize also that clarithromycin is probably a bad choice. Additionally an unacceptable high risk of acute renal failure due to the interaction between simvastatin and clarithromycin is visible in the ADR CP.
The situation looks much better meaning basically not changed compared to the scenario without antibiotic when looking at the ADR CPs with amoxicillin or cefaclor medications:
As the patient has no beta-lactam allergy Dr. Meyer is happy as he can quickly finish the clinical decision process and write the beta-lactam prescription for Willy Nottingham.
medication with Multaq/dronedarone, metoprolol, candesartan, simvastatin:
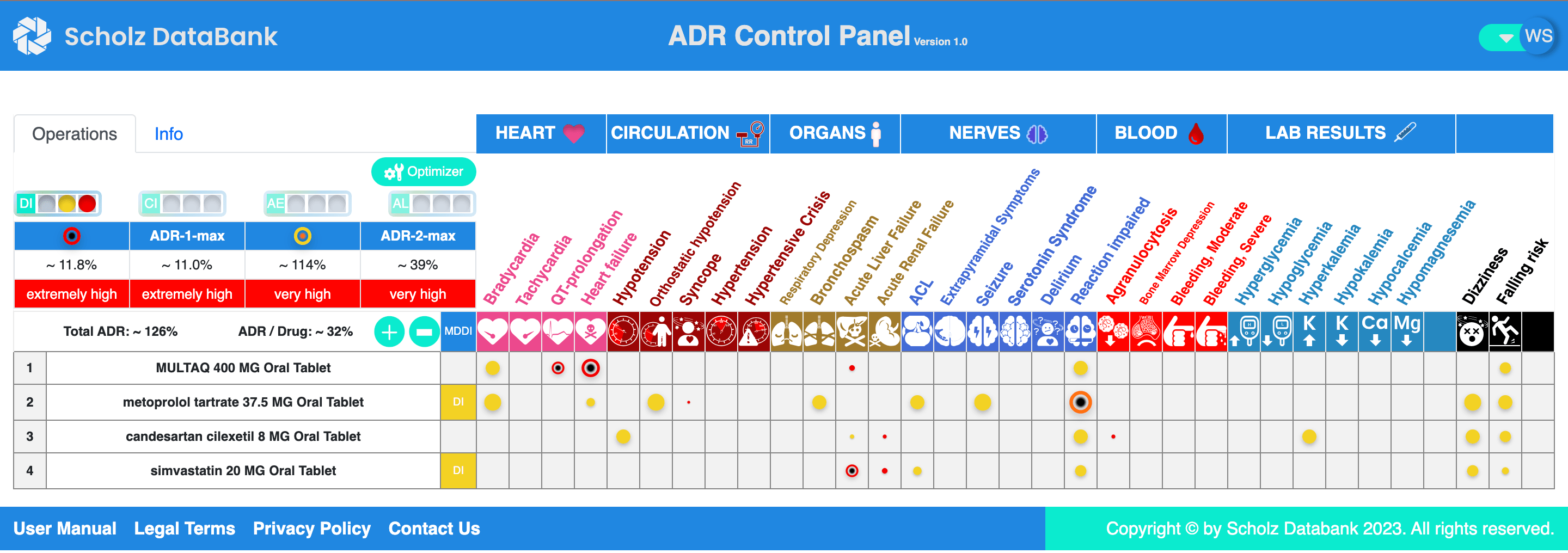
Dr. Meyer uses the ADR CP and is happy that he has stabilized the cardiovascular disease of Willy Nottingham with this medication and that he can overlook the major drug risks at one glance.
Willy Nottingham needs now an antibiotic due to a community acquired pneumonia diagnosed. Is clarithromycin appropriate? Or amoxicillin? Or Cefaclor? Is there any dangerous impact on the cardiac adverse risks which are already rather high and should not increase any more?
Dr. Meyer has abondened to waste his time working through long listings of pairwise potential drug drug interactions, for example when considering to prescribe clarithromycin.
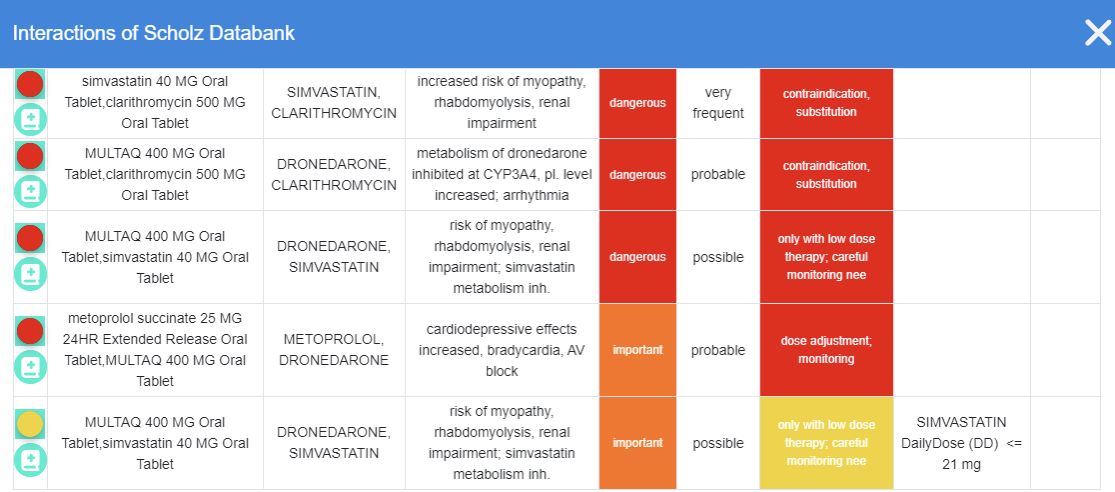
He just looks up and compares several ADR Control Panels without or with potential antibiotics to treat the pneumonia:
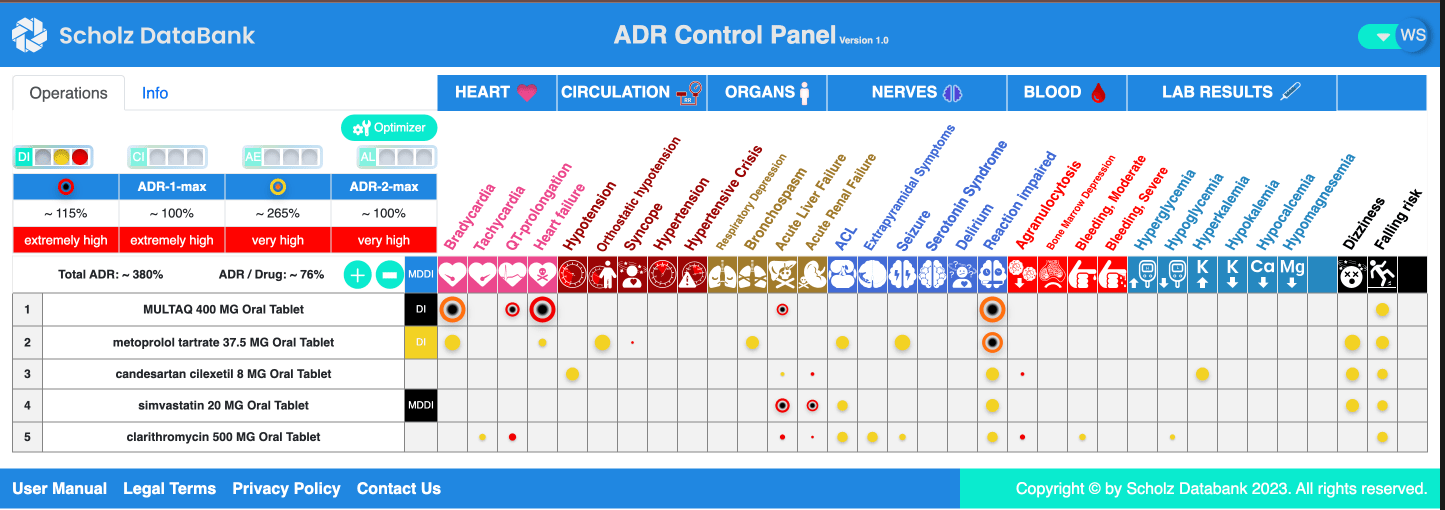
He realizes quickly the black MDDI alerts signalizing very hazardous kinetic drug drug interactions. The cardiac alerts for “QT prolongation” and “Heart Failure” emphasize also that clarithromycin is probably a bad choice. Additionally an unacceptable high risk of acute renal failure due to the interaction between simvastatin and clarithromycin is visible in the ADR CP.
The situation looks much better meaning basically not changed compared to the scenario without antibiotic when looking at the ADR CPs with amoxicillin or cefaclor medications:
As the patient has no beta-lactam allergy Dr. Meyer is happy as he can quickly finish the clinical decision process and write the beta-lactam prescription for Willy Nottingham.